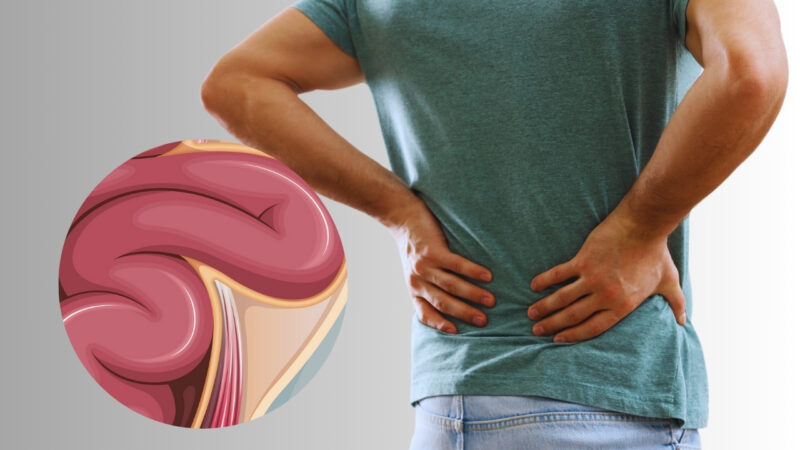
Hernias are commonly associated with discomfort in the abdominal or groin regions, but can they affect your back?
The simple answer is yes. Some hernias can indeed cause back pain by compressing or irritating nearby nerves.
For example, a herniated disc in the spine can pinch nerves and lead to radiating pain in the back, making daily tasks challenging. Recognizing these signs early on can help you seek appropriate treatment and alleviate your discomfort.
Consulting a healthcare professional is crucial if you suspect a hernia is affecting your back. They can perform a thorough evaluation to diagnose the issue properly.
1. Definition and Types of Hernias
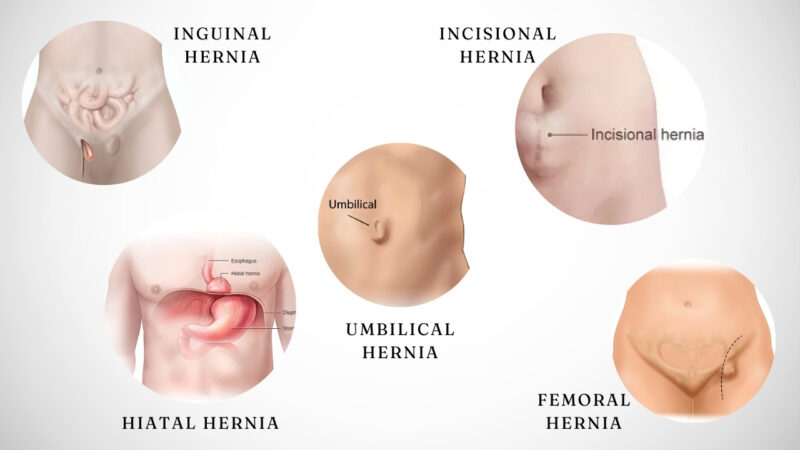
A hernia happens when an internal part of the body pushes through a weakness in the muscle or surrounding tissue wall according to NHS. There are several types of hernias:
- Inguinal Hernia: Occurs in the groin area, more common in men.
- Hiatal Hernia: Involves the stomach pushing up into the chest through the diaphragm.
- Umbilical Hernia: Happens near the belly button, commonly seen in infants.
- Incisional Hernia: Develops at the site of previous surgery.
- Femoral Hernia: Found just below the groin, mainly in women.
Common Causes of Hernias
- Physical strain such as heavy lifting or intense coughing can weaken muscle tissue, leading to hernias.
- Aging is another contributor, as muscles naturally weaken over time.
- Injury or surgery sites are more susceptible because the tissue has been disturbed or weakened.
- Genetic predisposition also plays a role; some people are inherently more likely to develop hernias.
- Obesity increases pressure on abdominal muscles, raising the risk.
- Finally, conditions like chronic constipation or persistent cough can increase intra-abdominal pressure, making a hernia more likely. .
2. Direct and Indirect Effects on the Back

For instance, a herniated disk can lead to significant back pain by pressing directly on the spinal nerves accoridng to NCBI.
This pressure can cause sharp, sometimes debilitating pain that radiates from your lower back to your legs.
In other cases, a hiatal hernia can indirectly affect your back.
This type of hernia places pressure on the diaphragm and surrounding tissues, leading to referred pain that might manifest in the back.
These effects are typically less immediate but can still cause chronic discomfort if not addressed.
Anatomical Considerations
Spinal hernias, such as herniated disks, are often the primary culprits behind back pain due to their direct interaction with spinal structures. Nerve pathways and muscle groups in the back are highly interconnected, making them susceptible to pressure and strain as per NCBI.
A lumbar hernia near the lower spine can compromise your posture and mobility, leading to additional muscle strain as your body adjusts to the discomfort according to Physiopedia.
Awareness of how different hernias affect anatomical structures can guide effective treatment and pain management strategies. Understanding these dynamics is key for addressing both the direct and indirect pain caused by hernias.
3. Diagnosis of Hernias

You may be asked to cough or strain, actions that help the hernia become more visible. Tenderness is another key indicator.
Inguinal and umbilical hernias are easier to detect through physical examination. Your doctor might also check for redness, swelling, or signs of tissue entrapment, which can indicate more severe cases.
Soldier-like attention to detail ensures that subtle signs are not missed, providing a more accurate initial diagnosis.
4. Imaging Techniques
Ultrasound is commonly used, especially for softer tissues like the abdomen.
CT scans and MRIs offer detailed, high-resolution images, crucial for detecting deeper or more complicated hernias according to sources. These methods are invaluable for assessing hernias in regions like the diaphragm.
Each technique has its specific use case and offers different insights. For example, a CT scan provides a comprehensive view to identify trapped tissues, while an ultrasound is less invasive and more convenient for initial evaluations.
5. Treatment Options

Surgical Interventions
The most common surgical procedures include open hernia repair and laparoscopic surgery.
Open hernia repair involves making an incision over the hernia site and returning the protruding tissue to its original position. The weakened area is then reinforced with stitches and sometimes a synthetic mesh to prevent recurrence according to Kenneth R. Hassler.
Laparoscopic surgery is minimally invasive and involves small incisions. A laparoscope, a thin tube with a camera, guides the surgeon. This method often results in shorter recovery times and less postoperative pain compared to open repair.
It’s important to address hernia pain promptly, as delaying treatment can lead to complications.
In some cases, robotic-assisted surgery may be employed to enhance precision. Discussing these options with your healthcare provider can help determine the best approach for your specific condition.
6. Non-Surgical Management
- Lifestyle changes play a significant role. Maintaining a healthy weight reduces abdominal pressure, lessening hernia symptoms.
- Wearing a truss or support garment can provide temporary relief, especially during activities that exacerbate discomfort. These garments apply gentle pressure to keep the hernia in place.
- Physical therapy and core-strengthening exercises help strengthen the abdominal muscles, providing better support and potentially alleviating some symptoms. However, you should perform these exercises under professional supervision to avoid worsening the hernia.
- Pain management techniques such as over-the-counter pain relievers or prescription medications may help control discomfort. Always consult healthcare professionals before starting any treatment regimen to ensure it aligns with your health needs.
7. Prevention and Risk Management
- Maintain a healthy weight: Excess body weight adds pressure to the abdominal area, increasing the risk of hernias. Aim for a balanced diet and regular exercise.
- Quit smoking: Smoking can hinder the healing process and weaken the abdominal muscles.
- Avoid heavy lifting: Use proper techniques or seek assistance to prevent straining your abdominal muscles.
Post-Surgery Care
After hernia surgery, follow these guidelines to avoid recurrence:
- Rest adequately: Allow your body to recover by avoiding strenuous activities for several weeks.
- Support your abdomen: Consider an abdominal belt to support the healing muscles.
- Follow medical advice: Adhere strictly to your doctor’s instructions on post-operative care.
Regular Exercise
Core strengthening exercises can help, but avoid movements that can strain your abdomen:
- Walking: Gentle walking can improve circulation and aid recovery without straining your abdominal muscles.
- Leg lifts and stretches: These low-impact exercises can strengthen your core gradually.
Dietary Choices
High-fiber foods ease digestion and prevent constipation, which can strain the abdomen:
- Fruits and vegetables: Incorporate plenty of fiber-rich fruits and vegetables in your diet.
- Whole grains: Opt for whole grains like oats, brown rice, and whole wheat.
Medical Consultations
- Regular check-ups: Regular visits to your healthcare provider can catch any early signs of a hernia.
- Seek immediate care: If you experience unusual symptoms or if a previously treated hernia reappears, consult your doctor promptly.
8. Diet and Nutrition

A balanced diet is essential for managing a hernia. Incorporating high-fiber foods, like fruits, vegetables, and whole grains, helps prevent constipation, which can strain the abdominal area and worsen the hernia according to some sources.
Staying hydrated is also crucial. Drinking plenty of water facilitates smooth digestion. Limiting foods that cause bloating and gas, such as beans, carbonated drinks, and fatty foods, can also reduce abdominal pressure and discomfort.
Maintaining a healthy weight through a proper diet reduces the stress on your abdomen and decreases the risk of hernia complications.
9. Potential Complications
Chronic pain is a common complication associated with hernias. This pain can persist even after surgical repair, affecting your activities and sleep. The severity and location of the pain often depend on the type and location of the hernia.
Inguinal hernias, for instance, may cause persistent discomfort in the groin area. Hiatal hernias can lead to pain in the upper abdomen and chest, sometimes radiating to the back. This pain may result from nerve irritation or muscle strain caused by the hernia.
Managing chronic pain often requires a combination of treatments, such as medication, physical therapy, and sometimes additional surgical interventions.
Implications for Mobility

Hernias can also impact your mobility, especially if they are left untreated. The discomfort and pain caused by a hernia can make it difficult to perform everyday activities, such as lifting objects, bending, or even walking.
For example, an abdominal hernia may cause pain when you cough, strain, or move suddenly. This can limit your ability to engage in physical activities, leading to muscle weakness and reduced overall fitness.
Surgical repair can improve mobility but may also involve a recovery period with limitations on physical activity. You may need to follow specific post-operative guidelines to ensure proper healing and avoid recurrence.
Related Posts:
- Weight Loss After Gallbladder Removal Surgery –…
- The Risks of Back Surgery - What You Need to Know…
- What is Incarcerated Hernias? - Causes, Symptoms,…
- How Stress and Anxiety Can Lead to Gastritis - What…
- What Is the Altemeier Procedure for Anastomosis? -…
- Signs of Parasitic Infections - 10 Key Symptoms Explained