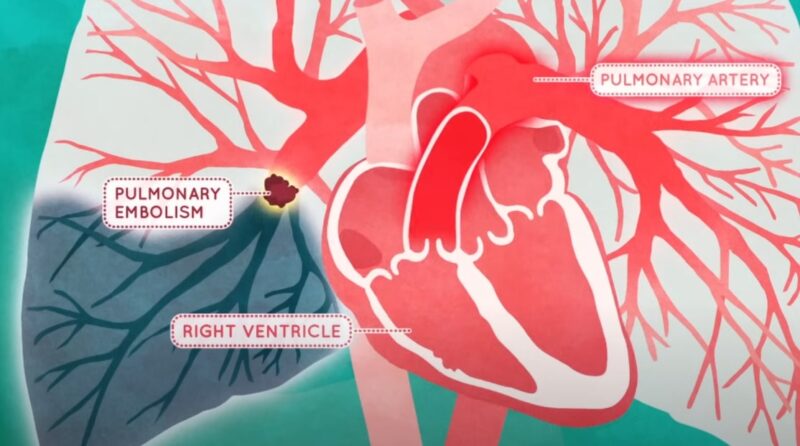
Deep vein thrombosis (DVT) is a serious condition where a blood clot forms in one of the deep veins, typically in the legs. This can lead to severe complications, including pulmonary embolism if the clot dislodges and travels to the lungs.
Recognizing and treating DVT promptly is crucial to prevent life-threatening outcomes. Treatment options vary based on the severity and location of the clot, ranging from anticoagulant medications to more invasive procedures. Understanding the available treatments is essential for managing this condition effectively and reducing the risk of future clots.
Key Takeaways
- Early recognition and prompt treatment of DVT are essential to prevent severe complications like pulmonary embolism.
- Treatment options vary from anticoagulant therapy to surgical interventions, tailored to the severity of the clot and patient-specific factors.
- Long-term management, including lifestyle changes and regular monitoring, is key to preventing recurrence and minimizing long-term effects.
Common Symptoms of DVT
Deep vein thrombosis (DVT) is often characterized by specific symptoms that can range from mild to severe. Recognizing these symptoms early is crucial, as prompt treatment can prevent serious complications like pulmonary embolism. Below is a detailed explanation of the most common symptoms associated with DVT.
1. Swelling in the Affected Leg

Swelling is one of the most noticeable symptoms of DVT. It usually occurs in one leg, although it can affect both in rare cases. The swelling is typically persistent and may increase over time, especially if the clot is large or located deep within the vein. The swelling results from the blockage of blood flow, causing fluid to accumulate in the tissues.
2. Pain or Tenderness
Pain or tenderness in the leg, particularly in the calf or thigh, is another common symptom. The pain often starts as a cramp or soreness and can gradually worsen. It may feel more pronounced when walking, standing for long periods, or flexing the foot upwards. This pain is caused by the pressure build-up in the vein due to the obstructed blood flow.
3. Warmth in the Skin
The skin over the affected area may feel warm to the touch. This warmth is a result of increased blood flow to the area as the body attempts to bypass the blockage. It is often accompanied by other symptoms such as redness and swelling, making it a key indicator of DVT.
4. Red or Discolored Skin
The skin over the area of the clot may appear red or discolored. In some cases, the entire leg may develop a bluish or purplish hue, which indicates poor circulation. This symptom occurs due to the restricted blood flow and the pooling of blood in the veins.
5. Visible Veins

In some cases, veins near the surface of the skin may become more visible or appear enlarged. This occurs as the body attempts to reroute blood around the clot, leading to increased pressure in nearby veins. These veins may become swollen and are often accompanied by tenderness.
6. Fatigue or Heaviness in the Leg
Many individuals with DVT report a feeling of heaviness or fatigue in the affected leg. This sensation is due to the increased effort required by the body to circulate blood past the clot. The leg may feel tired even after minimal activity, which can be a subtle but important symptom of DVT.
7. Leg Pain While Flexing the Foot
Pain that intensifies when flexing the foot upward, known as Homan’s sign, can be indicative of DVT. However, this is not a definitive test, as not all individuals with DVT will experience this symptom, and it can also be present in other conditions.
When to Seek Medical Attention
It’s essential to seek medical attention immediately if you experience any of these symptoms, especially if they develop suddenly. DVT can lead to life-threatening complications like pulmonary embolism, where a clot breaks loose and travels to the lungs. Early diagnosis and treatment are critical to prevent such outcomes.
For a detailed examination, doctors may use diagnostic tools like ultrasound, blood tests, and in some cases, venography, to confirm the presence of a clot and determine its severity. Once diagnosed, treatment will typically involve anticoagulant medications, lifestyle changes, and possibly more invasive procedures depending on the case.
Risk Factors for DVT
Understanding the risk factors for deep vein thrombosis (DVT) is essential for both prevention and early detection. While DVT can develop in anyone, certain conditions, lifestyle choices, and genetic predispositions can significantly increase the likelihood of forming a blood clot. Below are detailed explanations of the most common risk factors associated with DVT.
1. Prolonged Immobility

One of the primary risk factors for DVT is extended periods of immobility. This can occur during long flights or car rides, hospitalization, or recovery from surgery. When the legs are inactive for long periods, blood flow slows down, which increases the risk of clot formation. Individuals who are bedridden or have limited mobility due to medical conditions are particularly susceptible.
2. Surgery and Trauma
Surgical procedures, especially those involving the legs, hips, or abdomen, increase the risk of DVT. The trauma to blood vessels during surgery can trigger clot formation. Additionally, general anesthesia used during surgery can slow blood flow. Traumatic injuries, such as fractures, can also lead to DVT as the body responds to the injury by increasing clotting factors.
3. Pregnancy
Pregnancy is a significant risk factor for DVT due to increased pressure on the pelvic veins and changes in blood composition that favor clotting. The risk continues during the postpartum period, particularly in the first six weeks after delivery. Women with a history of DVT or certain clotting disorders are at even higher risk during pregnancy.
4. Hormone Therapy and Birth Control Pills
Hormone replacement therapy and certain types of birth control pills containing estrogen can increase the risk of DVT. These medications affect the balance of clotting factors in the blood, making it more prone to clotting. Women who smoke or have additional risk factors may have an even higher likelihood of developing DVT when using these medications.
5. Cancer and Cancer Treatment
Cancer, especially cancers of the pancreas, lungs, and brain, can increase the risk of DVT. Some types of chemotherapy, as well as the cancer itself, can lead to changes in blood composition, making clots more likely. Additionally, patients with cancer may be less mobile, further increasing their risk.
6. Inherited Blood Clotting Disorders
Certain genetic conditions can make blood more likely to clot. These include Factor V Leiden mutation, prothrombin gene mutation, and deficiencies in proteins like antithrombin, protein C, or protein S. Individuals with these inherited conditions have a significantly higher risk of developing DVT, especially when combined with other risk factors.
7. Age and Obesity
The risk of DVT increases with age, particularly after the age of 60. Aging veins and reduced physical activity can contribute to the development of clots. Obesity is another risk factor, as excess weight can increase pressure on the veins in the legs and slow blood flow. Additionally, obesity is often associated with other risk factors such as immobility and chronic medical conditions.
8. Smoking
Smoking has been linked to an increased risk of DVT as it affects blood circulation and clotting mechanisms. The chemicals in tobacco smoke can damage blood vessels and make blood more prone to clotting. The risk is compounded when smoking is combined with other factors like hormone therapy or a sedentary lifestyle.
9. Chronic Medical Conditions
Certain chronic conditions, such as heart disease, respiratory disorders, and inflammatory diseases, can increase the risk of DVT. These conditions often lead to decreased mobility, which slows blood flow and heightens the likelihood of clot formation.
10. Previous History of DVT or Pulmonary Embolism
Individuals who have previously experienced DVT or pulmonary embolism are at a higher risk of recurrence. This risk persists even after completing treatment, making ongoing monitoring and preventive measures essential.
Diagnosing DVT – What to Expect?
Diagnosing deep vein thrombosis (DVT) involves a combination of medical history, physical examination, and specific diagnostic tests. A healthcare provider will assess your symptoms and risk factors before conducting tests to confirm the presence of a clot.
1. Ultrasound
The most common and non-invasive test for DVT is a Doppler ultrasound. It uses sound waves to visualize blood flow in the veins and can detect blockages caused by clots.
2. D-Dimer Test
A D-dimer blood test measures a substance released when a blood clot breaks up. Elevated levels suggest the possibility of DVT, though other conditions can also cause high D-dimer levels.
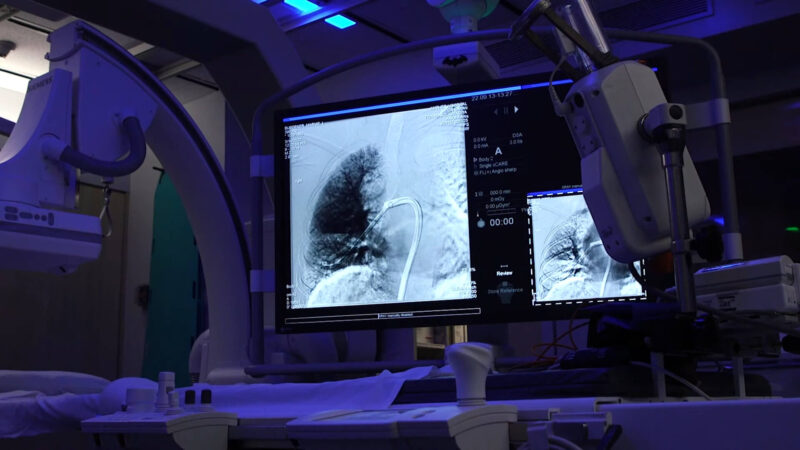
3. Venography
If ultrasound results are inconclusive, venography may be performed. This involves injecting a contrast dye into a large vein in your foot or ankle and taking X-rays to see the flow of blood and identify any clots.
4. Other Imaging Tests
In some cases, additional imaging tests like MRI or CT scans may be used, especially if the clot is in a location that’s difficult to assess with ultrasound.
Anticoagulant Therapy – The First Line of Defense
Anticoagulant therapy is the cornerstone of DVT treatment, aimed at preventing the clot from growing larger and reducing the risk of new clots forming. This therapy involves using blood-thinning medications, which can be administered orally or via injection.
1. Oral Anticoagulants

Common oral anticoagulants include warfarin and newer agents like apixaban, rivaroxaban, and dabigatran. These medications require regular monitoring, especially in the case of warfarin, to ensure the blood’s clotting ability remains within a safe range.
2. Injectable Anticoagulants
Heparin and low molecular weight heparins (LMWH) are often used initially to stabilize the patient. They are typically administered via injection and act quickly to prevent the clot from worsening.
3. Duration of Treatment
The duration of anticoagulant therapy depends on the individual’s risk factors and whether this is their first episode of DVT. Treatment usually lasts for three to six months but may continue longer in high-risk patients.
4. Monitoring and Side Effects
Patients on anticoagulants must be vigilant for signs of excessive bleeding, a common side effect. Regular blood tests are required to monitor the therapy’s effectiveness and adjust dosages as needed.
Thrombolytic Therapy for Severe Cases
Thrombolytic therapy, also known as clot-busting treatment, is used in severe cases of deep vein thrombosis (DVT) where rapid dissolution of the clot is necessary. This treatment is typically reserved for situations where there is a significant risk of complications, such as when a large clot threatens to block blood flow entirely or when there is a high risk of pulmonary embolism.
1. Administration Method
Thrombolytics can be administered intravenously or directly at the site of the clot through a catheter. The catheter-directed approach is often preferred to minimize systemic side effects and to deliver the drug more precisely to the clot.
2. Common Thrombolytic Agents
Medications used in thrombolytic therapy include alteplase (tPA), streptokinase, and urokinase. These agents work by breaking down the fibrin mesh that holds the clot together, effectively dissolving it.
3. Risks and Considerations
While thrombolytic therapy can be life-saving, it carries a significant risk of bleeding, including potentially fatal internal hemorrhaging. Because of these risks, this treatment is only considered when the benefits clearly outweigh the dangers.
4. Monitoring and Aftercare
Patients undergoing thrombolytic therapy require close monitoring in a hospital setting to manage any complications and to transition to anticoagulant therapy once the clot has been sufficiently reduced.
The Role of Compression Stockings in DVT Management
Compression stockings are a key component in the management and prevention of deep vein thrombosis (DVT). These specially designed stockings apply pressure to the legs, promoting better blood flow and reducing the risk of clot formation.
1. How Compression Stockings Work

Compression stockings exert graduated pressure on the legs, with the highest pressure at the ankles and gradually decreasing up the leg. This pressure helps to compress the veins, improve circulation, and prevent blood from pooling in the lower extremities, which is a major factor in clot formation.
2. When to Use Compression Stockings
These stockings are often recommended for individuals who are at high risk of developing DVT, such as those who have recently undergone surgery, are on long flights, or have a history of blood clots. They are also used in patients who have already been diagnosed with DVT to prevent further clots and reduce symptoms like swelling and pain.
3. Types of Compression Stockings
There are different types of compression stockings available, varying in strength (measured in mmHg) and length (knee-high, thigh-high, or full-length). The appropriate type is usually determined by a healthcare provider based on the patient’s specific needs and condition.
4. Benefits Beyond DVT Prevention
In addition to preventing DVT, compression stockings can help alleviate symptoms associated with chronic venous insufficiency and reduce the risk of post-thrombotic syndrome, a long-term complication that can occur after a DVT.
5. Considerations for Use
Proper fitting is crucial for the effectiveness of compression stockings. Ill-fitting stockings may not provide adequate compression or could cause discomfort. It’s also important to wear them consistently, particularly during the day when you are most active, and follow your healthcare provider’s recommendations on duration of use.
Surgical Interventions – When Clot Removal Is Necessary?
In certain cases of deep vein thrombosis (DVT), surgical intervention may be required to physically remove the blood clot, especially when other treatments are ineffective or the clot poses an immediate threat to health.
1. Thrombectomy
A thrombectomy is a surgical procedure in which the clot is directly removed from the vein. This is usually performed in severe cases where the clot is large or causing significant obstruction of blood flow. The surgery involves making an incision over the affected vein, accessing the clot, and carefully extracting it. Thrombectomy is often considered when there’s a risk of the clot breaking off and causing a pulmonary embolism.
2. Catheter-Directed Thrombolysis
Another surgical option is catheter-directed thrombolysis. In this procedure, a catheter is inserted into the vein and guided to the site of the clot. Through the catheter, clot-dissolving medication (thrombolytic agents) is directly administered to the clot, breaking it down. This method allows for a more targeted approach with less risk of systemic bleeding compared to intravenous thrombolysis.
3. Inferior Vena Cava (IVC) Filter Placement
For patients who cannot take anticoagulants due to bleeding risks, an IVC filter may be placed in the large vein (inferior vena cava) to catch clots before they reach the lungs. This filter is inserted via a catheter and acts as a physical barrier, preventing large clots from traveling to critical organs.
4. Risks and Considerations
Surgical interventions, while effective, come with their own set of risks, including infection, bleeding, and damage to the vein. These procedures are typically reserved for cases where the benefits outweigh the potential complications. Recovery time can vary depending on the procedure and the patient’s overall health.
5. Post-Surgical Care
After surgery, patients are closely monitored and may require anticoagulant therapy to prevent new clots from forming. Compression stockings and lifestyle changes are also recommended to support recovery and prevent recurrence.
FAQs
What are the long-term effects of DVT?
Long-term effects of DVT can include post-thrombotic syndrome (PTS), which occurs when the vein’s valves are damaged by the clot. Symptoms of PTS include chronic pain, swelling, and skin changes in the affected leg. In severe cases, it can lead to venous ulcers. Managing DVT effectively and following prescribed treatments can reduce the risk of these long-term complications.
Can DVT reoccur after treatment?
Yes, DVT can reoccur after treatment, especially if underlying risk factors are not managed. Individuals with a history of DVT are at a higher risk of recurrence. Continuous anticoagulant therapy, lifestyle modifications, and regular medical follow-ups can help prevent reoccurrence.
How does travel affect the risk of DVT?
Prolonged immobility during long flights or car rides can increase the risk of DVT. The lack of movement slows blood flow, particularly in the legs, which can lead to clot formation. To reduce the risk, it’s recommended to stay hydrated, move around frequently, and consider wearing compression stockings during long trips.
What lifestyle changes can help prevent DVT?
Lifestyle changes that can help prevent DVT include regular exercise, maintaining a healthy weight, quitting smoking, and staying hydrated. For those at higher risk, wearing compression stockings and avoiding prolonged immobility can also be beneficial. These changes improve overall circulation and reduce the likelihood of clot formation.
Are there any dietary considerations for managing DVT?
Certain foods, particularly those high in vitamin K (such as leafy greens), can affect the effectiveness of anticoagulant medications like warfarin. It’s important to maintain a consistent intake of vitamin K and discuss dietary habits with your healthcare provider. Staying hydrated and avoiding excessive alcohol can also support overall cardiovascular health and DVT management.
Last Words
In conclusion, deep vein thrombosis (DVT) is a serious condition that requires prompt attention and comprehensive management to prevent life-threatening complications. Recognizing the symptoms early and understanding the risk factors are crucial steps in preventing and treating DVT.
A variety of treatment options are available, from anticoagulant therapy and thrombolytic treatment to the use of compression stockings and surgical interventions, each tailored to the severity and specific circumstances of the patient.
Related Posts:
- What Causes a Vein to Burst in Your Leg and How to…
- How Effective Are Online Pharm.D. Programs Compared…
- What is Incarcerated Hernias? - Causes, Symptoms,…
- Contracted Gallbladder-Diagnosis and Treatment!
- Gallbladder Calculus and Acute Cholecystitis -…
- What Not to Do After Sclerotherapy? Post-Treatment Guideline