Taking care of your digestive health is no small feat, and when symptoms arise that require a closer look, it can be overwhelming to figure out which test is right for you.
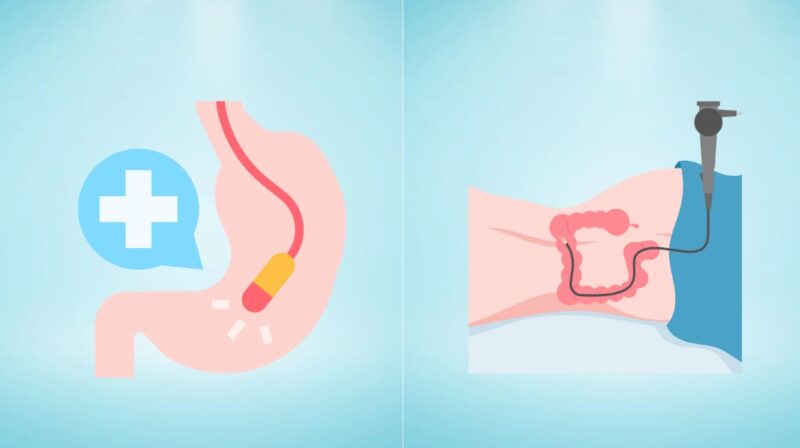
Lower endoscopies and colonoscopies are two common procedures used to investigate a variety of gastrointestinal (GI) issues. They may sound similar, but their purposes, scopes, and the experience they offer are quite different.
Let me share some insights to help you decide which procedure might suit your needs. I’ve had my fair share of conversations with healthcare providers and have learned that knowing what to expect helps you make informed choices.
What Is a Lower Endoscopy?
Lower endoscopy, often referred to as flexible sigmoidoscopy, gives your doctor a peek into the lower portion of your colon. Picture a flexible tube, equipped with a small camera, being guided into your rectum.
The goal? To check for inflammation, bleeding, or unusual growths like polyps. It’s a shorter journey compared to a colonoscopy, but it can still provide valuable information, especially if your symptoms are focused in the lower part of your abdomen.
What Happens During a Lower Endoscopy?
According to Clyde M. Stauffer, the procedure focuses on the sigmoid colon and rectum, offering a narrower view compared to its counterpart. Your doctor may suggest a lower endoscopy if you’ve been dealing with issues like:
- Chronic diarrhea
- Rectal bleeding
- Abdominal pain
- Conditions like ulcerative colitis or Crohn’s disease
Pros and Cons of Lower Endoscopy
While it’s quicker and less invasive, lower endoscopy doesn’t give the full picture. Its limited scope might not catch problems farther up the colon, so if there are concerns about areas outside the sigmoid colon, a colonoscopy might be more suitable.
What Is a Colonoscopy?
A colonoscopy is like the big brother of a lower endoscopy—it covers way more ground. In fact, it examines the entire colon, from the rectum all the way to the cecum, and sometimes even the end of the small intestine.
A colonoscopy is often the go-to for a more comprehensive check, especially if there are symptoms or concerns that suggest issues higher up in the GI tract.
When Is a Colonoscopy Recommended?
Your doctor may recommend a colonoscopy for a range of reasons, including:
- Persistent abdominal pain
- Changes in bowel habits
- Unexplained anemia or blood in the stool
- Family history of colorectal cancer
- Routine colorectal cancer screening (especially if you’re over 50)
According to Ervin Toth, unlike the lower endoscopy, a colonoscopy can examine the entire colon, which makes it ideal for not just diagnosing issues but also treating them.
The Process of a Colonoscopy
Let’s be honest—preparing for a colonoscopy isn’t fun. As the New England Journal of Medicine explains, it involves clearing out your entire colon, which means fasting and taking a laxative that will keep you glued to the bathroom.
But the upside is that sedation is usually provided, so you’ll be more comfortable during the procedure itself. The whole thing typically lasts around 30-60 minutes, though recovery may take a bit longer due to the sedation.
Comparing Lower Endoscopy and Colonoscopy

Let’s break it down side by side to make things clearer.
Scope of the Procedure
- Lower Endoscopy: Examines only the rectum and sigmoid colon.
- Colonoscopy: Examines the entire large intestine, from rectum to cecum, and sometimes even the small intestine.
Purpose
- Lower Endoscopy: Focuses on localized symptoms or monitoring known conditions in the lower GI tract.
- Colonoscopy: Used for more comprehensive evaluations, especially for colorectal cancer screening and broader diagnostic needs.
Preparation
- Lower Endoscopy: Easier prep, often just a small enema to clear the lower colon.
- Colonoscopy: Full bowel prep required, involving fasting and a laxative cleanse.
Invasiveness and Discomfort
- Lower Endoscopy: Less invasive, usually no sedation, but may cause discomfort like cramping.
- Colonoscopy: More invasive but typically done with sedation for a more comfortable experience.
Therapeutic Capabilities
- Lower Endoscopy: Can remove polyps or take biopsies, but only in the lower colon.
- Colonoscopy: Can remove polyps or take biopsies from the entire colon, making it more versatile for treatment.
Why Choose One Over the Other?

Deciding between a lower endoscopy and a colonoscopy depends on your symptoms, age, and medical history. Let’s take a look at some scenarios that might influence your choice.
Lower Endoscopy Might Be Right for You If:
- Your symptoms are localized to the lower part of your abdomen.
- You need monitoring for a specific condition like mild ulcerative colitis or Crohn’s disease.
- You want a less invasive procedure without full bowel prep or sedation.
Colonoscopy Might Be the Better Option If:
- You’re dealing with unexplained abdominal pain, anemia, or significant changes in bowel habits.
- You’re due for routine colorectal cancer screening, especially if you’re over 50 or have a family history of colorectal cancer.
- Your doctor wants a comprehensive view of your entire colon.
In simple terms, a lower endoscopy is a good option if you’re dealing with lower GI issues or you need something quick and less invasive.
Potential Risks and Complications

Both procedures are generally safe, but like all medical interventions, they aren’t completely risk-free.
Lower Endoscopy Risks
Since the procedure is less invasive, the risks are lower too. However, there’s a chance of bleeding or tearing at the biopsy or polyp removal sites. Cramping due to the air introduced into the colon is common but usually temporary.
Colonoscopy Risks
With colonoscopy, the risks are slightly higher because it’s a more extensive procedure. Complications can include perforation of the colon, bleeding, or sedation-related issues. While rare, they are still worth discussing with your doctor before the procedure.
What Should You Do Next?

The big question is: how do you decide which one is right for you? Start by having an open conversation with your healthcare provider. Let them know about any symptoms you’re experiencing, your medical history, and any concerns you have about the procedures.
Both lower endoscopies and colonoscopies play an important role in maintaining GI health. Lower endoscopies provide a focused look at the lower colon and are less invasive, while colonoscopies offer a full examination of the entire colon and are the gold standard for cancer screening.
Remember, every person’s situation is unique. What worked for a friend or family member may not be the best option for you.
Final Thoughts
At the end of the day, both procedures are key tools in catching GI issues early and providing peace of mind. Lower endoscopies might be easier in terms of preparation and recovery, but colonoscopies offer a more thorough examination, especially if there’s a need for a complete colon check.
Whichever route you end up taking, know that you’re taking an important step in keeping your digestive health in check. Trust the process, ask questions, and be sure to follow your healthcare provider’s guidance. Your body—and your peace of mind—will thank you for it.