Both types of hernias occur in the groin area, but they have distinct characteristics, causes, and risk factors that influence their diagnosis and treatment.
Direct inguinal hernias develop due to a weakness in the abdominal wall that typically arises with age or from physical strain, such as heavy lifting or chronic coughing. These hernias are more common in older adults and primarily affect men.
Indirect inguinal hernias, however, are often congenital. They occur when the inguinal ring does not close properly before birth. While they can appear at any age, they are frequently diagnosed in infants and children. Unlike direct hernias, indirect hernias can extend into the scrotum.
Recognizing the symptoms and understanding the risk factors can lead to timely and effective treatment. Both types of hernias may present with a noticeable bulge in the groin area, discomfort, and pain, especially during physical activities.
Key Takeaways
- Direct Inguinal Hernias occur due to a weakness in the abdominal wall that develops over time, typically affecting older adults and caused by physical strain or aging. They are located at the back wall of the inguinal canal and do not usually extend into the scrotum.
- Indirect Inguinal Hernias are often congenital, resulting from an incomplete closure of the inguinal ring present from birth. They follow the pathway that the testicles took during prebirth development, making them more likely to extend into the scrotum. They can appear at any age but are common in infants and children.
- Symptoms for both types include a noticeable bulge in the groin area, pain or discomfort, a heavy or dragging sensation, and swelling around the testicles if the intestine descends into the scrotum.
Overview of Inguinal Hernias
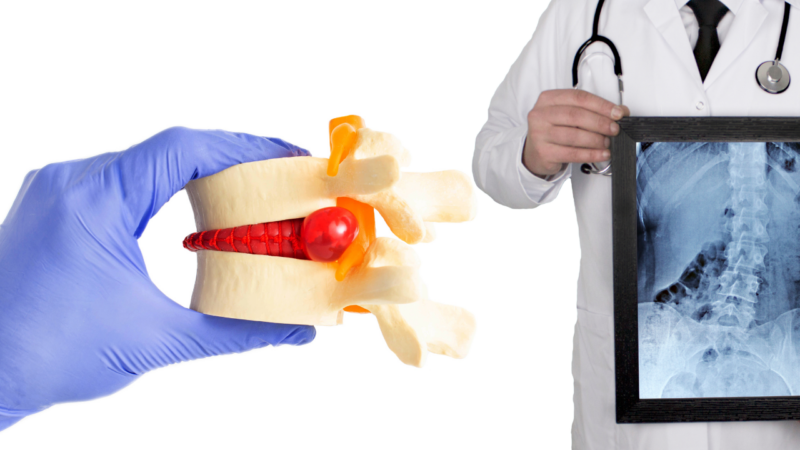
Inguinal hernias are one of the most common types of hernias and occur when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles. This condition results in a noticeable bulge in the groin area, which can cause discomfort and pain, especially during physical activities such as lifting, coughing, or bending.
Direct Inguinal Hernias
- Location: Occur at the back wall of the inguinal canal.
- Prevalence: More common in older adults, particularly men.
- Characteristics: These hernias do not usually extend into the scrotum and are often linked to activities that put stress on the abdominal muscles.
Indirect Inguinal Hernias
Indirect inguinal hernias are often congenital, meaning they are present from birth. They occur when the inguinal ring, a passage through the abdominal wall, fails to close properly during fetal development.
- Location: Follow the pathway that the testicles made during prebirth development, potentially extending into the scrotum.
- Prevalence: Common in infants and children, but can also appear later in life due to an acquired weakness.
- Characteristics: These hernias are more likely to extend into the scrotum compared to direct hernias.
Causes of Direct Inguinal Hernias
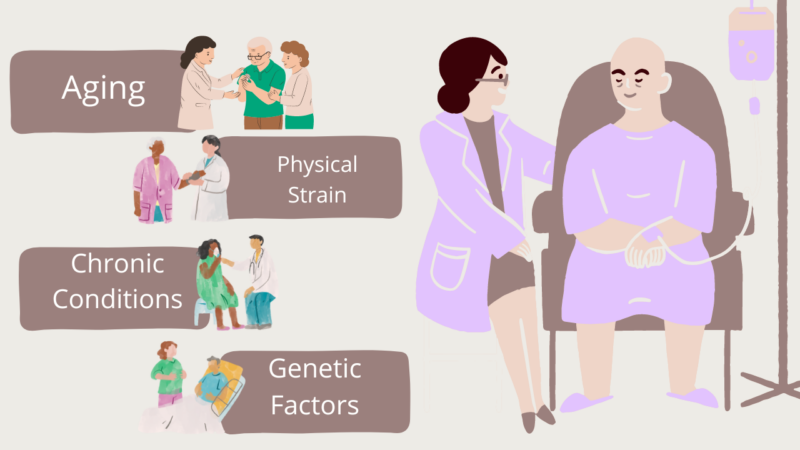
This weakness can develop over time and is often influenced by various factors:
- Aging: As people age, the muscles in the abdominal wall can become weaker and less resilient, making them more susceptible to herniation.
- Physical Strain: Activities that increase pressure in the abdomen, such as heavy lifting, chronic coughing, or straining during bowel movements, can contribute to the development of these hernias.
- Chronic Conditions: Conditions that lead to increased abdominal pressure, such as chronic obstructive pulmonary disease (COPD), constipation, or obesity, can also increase the risk.
- Genetic Factors: A family history of hernias can indicate a genetic predisposition to developing weak spots in the abdominal wall.
Causes of Indirect Inguinal Hernias
Indirect inguinal hernias are typically congenital, meaning they are present from birth. They occur when the inguinal ring, a passageway through the abdominal wall, does not close properly during fetal development.
Here are the primary causes:
- Congenital Defect: The most common cause is an incomplete closure of the inguinal ring, allowing abdominal contents to protrude through this weak spot.
- Genetic Predisposition: A family history of hernias can increase the likelihood of developing this condition, indicating a genetic component.
- Increased Abdominal Pressure: Factors such as heavy lifting, chronic coughing, or straining during bowel movements can exacerbate the condition and lead to hernia development.
Symptoms of Inguinal Hernias
Recognizing the symptoms is crucial for early diagnosis and treatment.
- Visible Bulge: A noticeable bulge in the groin or scrotum area that becomes more apparent when standing, coughing, or straining.
- Pain or Discomfort: A burning, gurgling, or aching sensation at the site of the bulge, especially during physical activities.
- Heaviness or Weakness: A feeling of heaviness, weakness, or pressure in the groin area.
- Occasional Swelling: Swelling around the testicles when the protruding intestine descends into the scrotum.
Treatment
Here are the primary treatment options:
- Open Surgery: Involves making a single large incision in the groin to push the protruding tissue back into place and repair the weak spot in the abdominal wall, often using a synthetic mesh for reinforcement. This method is effective and has a relatively quick recovery time.
- Laparoscopic Surgery: A minimally invasive procedure where several small incisions are made, and special instruments, including a camera, are used to repair the hernia from inside the abdomen. Mesh is usually used to strengthen the repair. Laparoscopic surgery generally offers quicker recovery and less postoperative pain compared to open surgery.
- Watchful Waiting: In cases where the hernia is small and not causing significant symptoms, doctors might recommend monitoring the condition closely and delaying surgery. This approach is less common due to the risk of complications over time.
Risks and Prevention
Here are the key risks and prevention strategies:
Main Risks
- Age: The risk of developing a hernia increases with age as the muscles in the abdominal wall weaken over time.
- Gender: Men are significantly more likely to develop inguinal hernias than women.
- Family History: A family history of hernias can indicate a genetic predisposition to developing this condition.
- Chronic Cough: Conditions that cause chronic coughing, such as smoking or respiratory illnesses, can increase abdominal pressure and the risk of hernia.
- Chronic Constipation: Straining during bowel movements can lead to increased pressure on the abdominal wall.
- Heavy Lifting: Regularly lifting heavy objects without proper technique can cause or exacerbate a hernia.
- Obesity: Excess weight increases the strain on the abdominal muscles, contributing to the risk.
- Previous Hernia: A personal history of hernias increases the likelihood of recurrence.
Prevention
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight reduces pressure on the abdominal wall.
- Proper Lifting Techniques: Use your legs rather than your back when lifting heavy objects to minimize abdominal strain.
- Avoid Straining: Treat conditions like chronic cough and constipation to prevent straining that can lead to hernias.
- Strengthen Abdominal Muscles: Regular exercise can help strengthen the muscles in the abdominal wall, providing better support and reducing the risk.
- Quit Smoking: Smoking cessation helps prevent chronic cough and improves overall muscle health.
Complications of Untreated Hernias
Incarceration
- Definition: Occurs when the herniated tissue becomes trapped and cannot be pushed back into the abdomen.
- Symptoms: Severe pain, nausea, vomiting, and a firm, tender bulge.
- Consequences: Can lead to bowel obstruction, causing significant discomfort and potential complications if not treated promptly.
Strangulation
- Definition: A life-threatening condition where the blood supply to the herniated tissue is cut off.
- Symptoms: Intense pain, redness over the hernia site, fever, and signs of sepsis.
- Consequences: Can cause tissue death and requires emergency surgery to prevent severe outcomes, including death.
Bowel Obstruction
- Definition: When the herniated intestine becomes obstructed.
- Symptoms: Abdominal pain, bloating, nausea, vomiting, and inability to pass gas or stool.
- Consequences: Requires urgent medical attention to relieve the obstruction and prevent further complications.
Chronic Pain
- Definition: Persistent pain in the groin area due to untreated hernia.
- Symptoms: Ongoing discomfort that can affect daily activities and quality of life.
- Consequences: Chronic pain can be debilitating and may require medical management or surgical intervention.
Infection
- Definition: An infection can develop if the herniated tissue becomes strangulated and starts to die.
- Symptoms: Redness, warmth, and swelling at the hernia site, fever, and chills.
- Consequences: Can lead to severe systemic infection (sepsis) requiring immediate medical treatment.
Available Surgeries
Surgical repair is the definitive treatment for inguinal hernias, preventing complications and providing relief from symptoms. The choice of surgical technique depends on factors such as the type of hernia, the patient’s health, and the surgeon’s expertise. Here are the primary surgical techniques:
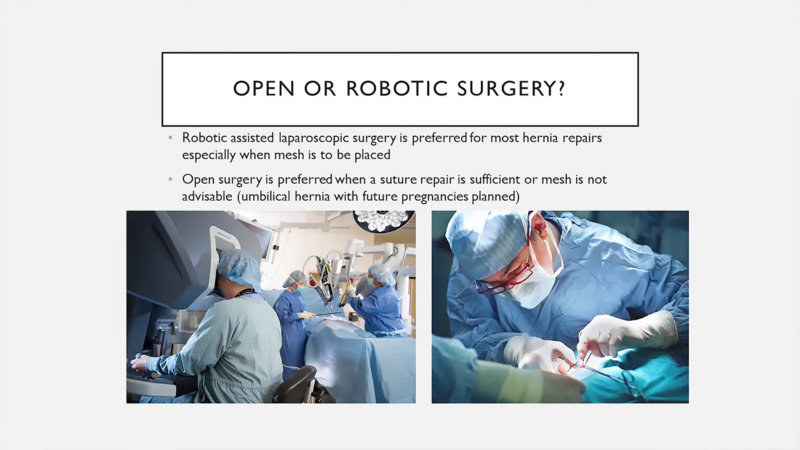
Open Surgery
- Procedure: The surgeon makes an incision directly over the hernia, pushes the protruding tissue back into the abdomen, and repairs the weak spot in the abdominal wall. Often, a synthetic mesh is used to reinforce the repair.
- Advantages: Generally considered straightforward and effective, especially for large hernias or in cases where laparoscopy is not suitable.
- Recovery: Patients typically experience a moderate recovery period, with most returning to normal activities within a few weeks.
Laparoscopic Surgery
- Procedure: The surgeon makes small incisions through which a laparoscope (a thin tube with a camera) and other surgical instruments are inserted. The hernia is repaired from the inside using mesh.
- Advantages: This method usually results in less postoperative pain, smaller scars, and a quicker return to normal activities compared to open surgery.
- Recovery: Patients often recover faster and with less discomfort, typically resuming normal activities within a week or two.
Robotic-Assisted Surgery
- Procedure: The surgeon controls robotic arms that provide greater dexterity and precision, making it easier to perform complex repairs through small incisions.
- Advantages: Offers high precision, minimal invasiveness, and potentially faster recovery with reduced postoperative pain.
- Recovery: Similar to laparoscopic surgery, patients usually experience a quick recovery period.
Mesh vs. Non-Mesh Techniques
- Mesh Repair: Mesh is placed over the weak spot to provide additional support and reduce the risk of recurrence. This method is widely used due to its effectiveness in preventing hernia recurrence.
- Non-Mesh Repair: In some cases, particularly in certain countries or when mesh is not available, non-mesh techniques are used. These involve stitching the muscle layers together, which may have higher recurrence rates compared to mesh repairs.
Post-Surgery Recovery and Care
- Recovery Period: Most patients can go home the same day as the surgery. Full recovery can take several weeks, depending on the type of surgery performed.
- Activity Restrictions: Patients are advised to avoid heavy lifting and strenuous activities during the recovery period to prevent strain on the repaired area.
- Follow-Up: Regular follow-up appointments are necessary to monitor the healing process and address any complications.
Recovery and Care
Here’s what you need to know about the post-surgery phase:
Immediate Post-Surgery Care

- Observation: After the surgery, patients are typically monitored in a recovery room for a few hours to ensure there are no immediate complications such as excessive bleeding or adverse reactions to anesthesia.
- Discharge: Most inguinal hernia surgeries are performed on an outpatient basis, meaning patients can usually go home the same day. However, someone should be available to drive the patient home and assist them initially.
Pain Management
- Medications: Pain and discomfort are common after hernia repair surgery. Doctors may prescribe pain medications or recommend over-the-counter pain relievers to manage this.
- Ice Packs: Applying ice packs to the surgical area can help reduce swelling and alleviate pain during the first few days post-surgery.
Activity Restrictions
- Rest: It’s crucial to get plenty of rest and avoid strenuous activities for the first few weeks after surgery. This helps prevent strain on the surgical site.
- Lifting Restrictions: Patients are advised to avoid heavy lifting (usually anything over 10 pounds) and intense physical activities for at least 4-6 weeks. Gradual reintroduction to normal activities is recommended.
- Walking: Gentle walking is encouraged as it promotes circulation and helps prevent blood clots. Start with short walks and gradually increase the distance as comfort allows.
Wound Care
- Incision Care: Keep the surgical site clean and dry. Follow the doctor’s instructions regarding bathing and changing dressings.
- Signs of Infection: Watch for signs of infection such as increased redness, swelling, warmth, or discharge at the incision site, as well as fever. Report any of these symptoms to a healthcare provider promptly.
Follow-Up Appointments
- Regular Check-Ups: Attend all scheduled follow-up appointments with the surgeon. These visits are essential for monitoring the healing process and addressing any concerns or complications.
- Monitoring: The surgeon will check the surgical site, discuss any symptoms, and provide guidance on when normal activities can be resumed.
Long-Term Care
- Activity Gradation: Gradually increase physical activity as advised by the healthcare provider. Returning to normal activities too quickly can increase the risk of hernia recurrence.
- Healthy Lifestyle: Maintaining a healthy weight, eating a balanced diet, and avoiding activities that increase abdominal pressure can help prevent future hernias.
Potential Complications
- Recurrence: There is a small risk of hernia recurrence even after surgical repair. Following post-surgery guidelines carefully can minimize this risk.
- Chronic Pain: Some patients may experience chronic pain at the surgical site. If this occurs, it’s important to discuss it with a healthcare provider for appropriate management.
Conclusion
Knowing the differences between direct and indirect inguinal hernias is crucial for proper treatment. Direct hernias often result from muscle weakness due to aging or physical strain and are more common in older men. Indirect hernias, usually present from birth, can show up at any age and often extend into the scrotum.
Both types cause similar symptoms like a visible bulge, pain, and discomfort in the groin area. Diagnosing these hernias usually involves a physical exam, and sometimes imaging tests. Surgery is often needed to fix the issue and prevent serious complications.
If you suspect you have a hernia, seek medical advice promptly to determine the best course of action and avoid potential health risks.
Related Posts:
- What is Ambulatory Surgery? - Everything You Need to Know
- Top 13 Healthcare Jobs That Don’t Know You Need Experience
- What’s Behind Gluten Sensitivity? 10 Causes You Need to Know
- Common Colonoscopy Questions: What You Need to Know
- The Risks of Back Surgery - What You Need to Know…
- How Stress and Anxiety Can Lead to Gastritis - What…