Medicare serves as a cornerstone of healthcare for millions of Americans, particularly those aged 65 and older.
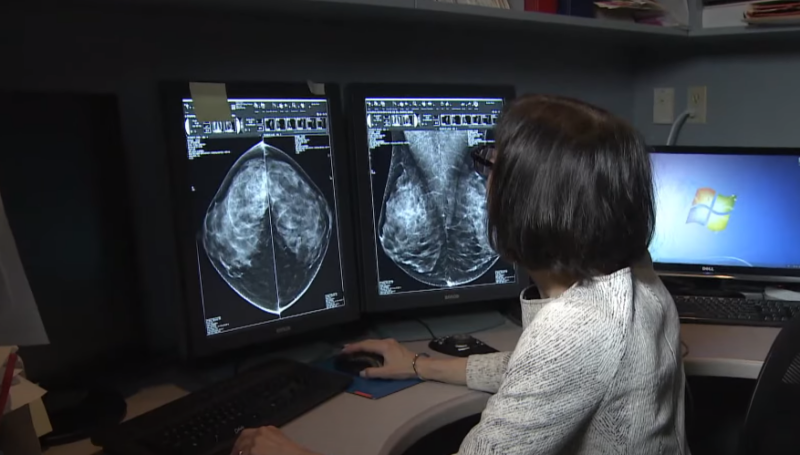
As medical technology advances and healthcare delivery evolves, outpatient surgery has become a common alternative to inpatient procedures, offering the convenience of same-day discharge and the potential for reduced costs.
We aim to demystify the costs associated with outpatient surgery under Medicare, providing insights into how beneficiaries can manage expenses without sacrificing the quality of their care.
Medicare Coverage

Medicare’s structure is composed of several parts, each with a specific focus.
| Medicare Part | Coverage Details |
|---|---|
| Part A | – Inpatient hospital stays – Skilled nursing facility care – Some home health visits |
| Part B | – Physician services
– Outpatient care – Preventive services (pertinent to outpatient surgery) |
| Part C (Medicare Advantage) | – Alternative way to receive Medicare benefits
– Provided through private insurance companies |
| Part D | – Prescription medications |
Supplemental insurance plans, known as Medigap, can be purchased to cover expenses not fully reimbursed by Medicare Parts A and B, such as copayments, coinsurance, and deductibles.
Medicare Payment for Outpatient Surgery
Medicare’s approach to covering outpatient surgery costs is both systematic and complex, designed to ensure that beneficiaries receive the necessary care while also controlling expenses.
The payment for these procedures is largely governed by the Outpatient Prospective Payment System (OPPS), which Medicare uses to determine the fixed rates for services provided in hospitals and ambulatory surgical centers.
Under the OPPS, payments are standardized based on the classification system known as Ambulatory Payment Classifications (APCs). Each APC groups together procedures that are similar in clinical nature and in terms of the resources they require.
Medicare then pays the facility a set fee for the entire group of services associated with a particular APC, regardless of the specific procedure performed or the individual variations in cost. This system is designed to simplify billing and create an incentive for facilities to provide cost-effective care.
The actual amount that Medicare will pay for a specific outpatient surgery can vary based on several factors. The type of surgery is a primary determinant, as more complex and resource-intensive procedures will fall under APCs with higher reimbursement rates.
The setting also matters; procedures performed in a hospital outpatient department may be reimbursed at a different rate than those done in an ambulatory surgery center. Additionally, beneficiaries are typically responsible for paying a portion of the Medicare-approved amount, including any applicable deductible and coinsurance.
For example, after meeting the annual Part B deductible, a beneficiary would usually pay 20% of the Medicare-approved amount for the doctor’s services. For the facility fee, Medicare will pay 80%, and the beneficiary is responsible for the remaining 20%, which can be covered by supplemental insurance or out-of-pocket payments.
Strategies for Cutting Costs

For Medicare beneficiaries, the quest to reduce out-of-pocket expenses is not just a matter of budgeting, but a strategic endeavor to maximize the value of their healthcare coverage.
While it provides a substantial framework for managing these costs, the onus is on the patients to explore and utilize various avenues that can lead to financial savings.
The strategies for cutting costs involve a proactive approach, from understanding the specifics of Medicare plans to making informed decisions about care providers.
Now we will name of the strategies you can utilize:
- Review and understand your Medicare plan details thoroughly.
- Consider the benefits of supplemental insurance to cover potential gaps.
- Explore different healthcare providers and facilities for competitive pricing.
- Utilize preventive services offered by Medicare to avoid more costly procedures.
- Inquire about the possibility of discounts or payment plans from healthcare providers.
- Stay informed about changes in Medicare policies that may affect surgery costs.
Navigating the System Without Cutting Corners
Quality care should never be compromised for the sake of cost.
Beneficiaries should work closely with their primary care physicians to coordinate their outpatient surgery, ensuring that all aspects of their care meet high standards. Understanding patient rights and how to advocate within the Medicare system is also key.
Resources such as the hotline and Medicare.gov provide valuable information and assistance.
What Does the Future Hold?

Technological advancements in medical procedures are expected to streamline operations and reduce the need for extensive hospital stays, potentially lowering costs. However, these innovations often come with high initial price tags, which Medicare must negotiate and manage.
The demographic shift with an aging population will likely increase the demand for outpatient services, prompting to adapt coverage policies. The interplay between adopting new technologies and managing a growing beneficiary base will be a significant factor in shaping Medicare’s approach to outpatient surgery costs.
Policy changes also loom on the horizon as lawmakers grapple with the sustainability of Medicare funding. Proposals to modify payment models, such as bundled payments for certain outpatient procedures, could incentivize cost savings and quality care.
The expansion of telehealth services, which has seen a rapid acceleration due to the pandemic, may become a permanent fixture in the outpatient landscape, offering potential cost reductions and increased access to care.
As Medicare evolves, it will need to balance cost containment with the provision of comprehensive, high-quality care, ensuring that beneficiaries can afford and access the outpatient services they need without undue financial burden.
FAQs
How can I find out if my outpatient surgery will require a copayment?
You can find out if a copayment is required by contacting your doctor, the facility where the surgery will be performed, or Medicare directly. The Medicare & You handbook also provides information on copayments for covered services.
Are follow-up treatments related to outpatient surgery covered by Medicare?
Follow-up treatments that are medically necessary are generally covered by Medicare. This includes post-operative visits, physical therapy, or any other follow-up care related to the surgery.
What options do I have if I cannot afford the out-of-pocket costs for outpatient surgery under Medicare?
If you’re having difficulty affording out-of-pocket costs, you may look into supplemental insurance plans like Medigap, programs like Medicaid, or assistance from charitable organizations.
How do I appeal a coverage decision by Medicare for an outpatient surgery?
To appeal a Medicare decision, you must first receive the Medicare Summary Notice (MSN) that explains why a claim was denied. The MSN includes instructions on how to appeal the decision, and you typically have 120 days after the date you receive the notice to file an appeal.
Summary
Understanding how Medicare covers outpatient surgery is crucial for beneficiaries looking to manage their healthcare expenses effectively.
By being well-informed, proactive in cost comparison, and engaged in their healthcare decisions, Medicare recipients can ensure they receive the necessary surgical care without undue financial hardship, maintaining the delicate balance between cost and quality.
If you are interested in similar topics, check our website.
Related Posts:
- How Much Does Aflac Pay for Outpatient Surgery: Find Out!
- Top 6 Money-Saving Tips on Prescription Medications…
- How Much Does a Wheelchair Cost?
- 10 Smart Ways to Cut Hospital Costs During Planned Surgery
- Outpatient Surgery vs. Inpatient Care: Which Is…
- What to Eat and What Not- After Appendix Removal Surgery