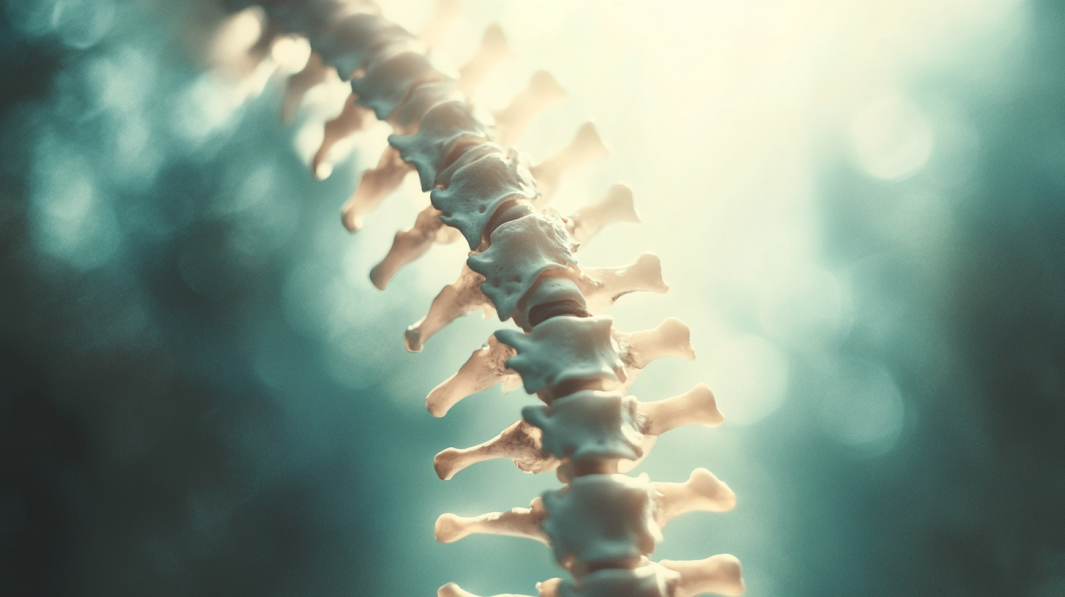
Spondylolisthesis is a condition where one vertebra slips over the one underneath it, which leads to aches and other complications.
There are two main types:
- Dysplastic; that’s congenital
- Isthmic; normally because of small pressure fractures
Spondylolisthesis has symptoms like returned pain and nerve compression, making it hard for sufferers to hold a very good excellent of life.
When conservative treatments fail, surgical procedure turns into a viable option for relief.
Let us talk about it.
Indications for Surgery
Surgery is usually considered when things like physical therapy, meds, or lifestyle changes stop easing symptoms.
Simple treatments try to manage pain, improve flexibility, and lower swelling.
But when they quit working, surgery may be the next step.
Getting Worse Over Time
One main reason for the operation is the slippage continues to get more severe. This condition could not only heighten pain but also lead to other issues.
As the bones keep sliding out of place, they can put extra pressure on nerves and tissues.
This tends to heighten discomfort, often meaning conservative methods aren’t enough anymore. In these cases, surgery may be needed to realign the back and halt further degeneration.
Increasing Aches
When pains persist or get worse despite non-surgical help, it may be clear that an operation is required.
For many patients, conservative methods like meds and physical therapy can ease symptoms at first, but as the condition progresses, the pain can become unbearable.
Surgery here focuses on stabilizing the spine and relieving pressure on nerves to lower pain.
Nerve Symptoms
Nerve symptoms, such as issues with the bladder or bowels, are serious signs nerve compression has escalated. These symptoms suggest the spondylolisthesis is squeezing the spinal nerves so much permanent harm could happen if left untreated.
At this stage, surgery is often necessary to prevent further nerve damage, ease nerve pressure, and restore regular function.
Reduced Quality
When spondylolisthesis greatly impacts someone’s quality of life-limiting mobility and daily activities—surgical involvement may be the best choice.
Simple remedies might ease symptoms for a while, but they may not fix the root problem.
The operation aims to realign the spine and reinforce it, to boost how the person feels in their daily life overall.
Surgical Procedures for Spondylolisthesis

Surgical treatment usually focuses on two main procedures: decompression surgery and spinal fusion. Both are meant to lessen issues and increase stability depending on how severe things are.
The goal is to give relief and support so folks can start feeling like themselves again.
Decompression Surgery (Laminectomy)
This operation is designed to ease pressure on spinal nerves by removing parts of bone or tissue causing compression. It is particularly effective for relieving symptoms such as:
- Leg pain
- Numbness
- Tingling caused by squeezed nerves
Spinal Fusion
The main goal of spinal fusion is to stabilize the backbones and prevent any further slipping out of place.
During this procedure, the surgical team will use bone grafts, rods, and screws to fuse two or more of the bones permanently.
A couple of different methods are commonly used for this part of the surgery:
- Anterior Lumbar Interbody Fusion (ALIF): Doctors access the spine from the front side.
- Transforaminal Lumbar Interbody Fusion (TLIF): Doctors reach the spine from the back or side.
The exact method chosen will depend on each person’s unique situation and what the lead surgeon feels is best based on their examination and experience.
In some situations, the surgical team may decide that instead of the regular fusion process, other choices could be a better fit. One example might be the Premia Spine TOPS System.
Minimally Invasive Surgery
This type of surgery is preferred for its advantages, such as:
- Smaller cuts
- Reduced tissue damage
- Speedier recovery times
However, in more complex cases involving severe slipping or instability, open surgery may be needed.
Considerations
The decision between decompression, spinal fusion, or a combination depends on:
- How bad the spondylolisthesis is
- The person’s overall health
The surgeon’s recommendations are based on images and the person’s situation.
Each procedure has its own risks and benefits, and the most suitable choice depends on the individual’s needs.
Common Risks and Complications

Like any operation, spondylolisthesis procedures carry potential risks and issues. Below are some of the most common complications:
Pseudoarthrosis (Non-Union)
One of the most frequent problems is pseudoarthrosis, or when the bones don’t fuse right after spinal fusion surgery.
This can lead to ongoing back instability and lingering pain, often requiring extra surgery.
Things like smoking, obesity, and severe slipping can raise the chances of pseudoarthrosis.
Nerve Complications
Nerve risks are a major concern, especially when nerves are squeezed. Damage to nerves during surgery can cause pain, weakness, or paralysis in bad cases.
High-grade slipping or aggressive surgical reductions increase the likelihood of these issues.
However, neuromonitoring – which provides real-time nerve feedback during surgery – helps reduce those risks.
Adjacent Segment Disease (ASD)
Another potential issue is adjacent segment disease. This occurs when the vertebrae directly above or below the fused part start deteriorating over time.
Long fusions can place extra strain on nearby bones, heightening degeneration risk. This condition can mean more operations to address new problems.
Additional Complications

In addition to the more common complications, several other risks are linked to spondylolisthesis surgery. While many of these issues are rare, patients need to be aware of them before undergoing the procedure.
Infection
As with any operation, there’s always a chance of infection, especially at the surgical site. Strict cleanliness steps and antibiotics are used to lower this risk. But infections can still happen and may need extra treatment.
Hardware Issues
Rods, screws, and other gear used during spinal fusion sometimes fail by breaking or loosening. This hardware problem can compromise the fusion site’s stability, leading to ongoing or worsening symptoms. In these cases, added surgery may be needed to address the issue.
Bleeding and Dural Tears
Bleeding is a standard risk for any operation. But it’s especially important for more invasive back surgeries. Tears in the membrane around the spinal cord can also occur, leading to fluid leakage from the brain and spine, possibly requiring more involvement.
Transition Syndrome
Transition syndrome arises when non-fused back areas experience increased strain due to stabilizing adjacent bones. Extra pressure can cause deterioration in previously unaffected regions, resulting in long-term discomfort and sometimes future operations.
Factors Increasing Complication Risks

Several factors can significantly elevate the risk of complications during spondylolisthesis surgery. While surgery can be successful for many, certain conditions and lifestyle factors can make the process more challenging.
Age
Age is one of the primary factors that affect surgical outcomes. Older patients face greater risks due to age-related complications, such as:
- Slower healing processes
- Reduced bone fusion effectiveness, increasing the risk of pseudoarthrosis or adjacent segment disease
- Elderly patients are more likely to have comorbidities such as:
- Heart disease
- Diabetes
- Osteoporosis
These conditions complicate both the surgery and the recovery process.
Lifestyle Factors
Some lifestyle habits also really matter for the risk of issues during or after surgery:
- Smoking: Lighting up stops bones from healing as well and raises the chances of infection or hardware problems.
- Weight: Extra pounds put more pressure on the back and increase the risk of bones not fusing together right or hardware complications.
Taking care of yourself makes a difference. Surgery is a big deal, so doing what you can to support a good outcome is important. Your health is worth maintaining so you can feel your best.
Osteoporosis
Patients with osteoporosis are particularly vulnerable to complications such as fractures during surgery. Their bones may be too fragile to achieve a successful fusion, further complicating the healing process.
Prior Surgeries

Individuals who have undergone previous back surgeries are at higher risk for complications. Key concerns include:
- Scar tissue, which can obscure visibility during surgery
- Greater difficulty in safely navigating around nerves and other critical structures
This can make a second surgery more challenging and increase the risk of nerve damage or other issues.
The Bottom Line
Operation for spondylolisthesis can really help with pain relief and boost the quality of life for many folks. Still, it’s key to grasp the risks and possible issues.
By paying attention to these factors and picking the right surgical method, patients can get better long-lasting results.
While surgery isn’t simple, understanding potential challenges can help people make informed choices and feel more prepared for success. I wish all dealing with this condition the very best in whatever path they choose.
Related Posts:
- The Risks of Back Surgery - What You Need to Know…
- What to Eat and What Not- After Appendix Removal Surgery
- First Time Under the Knife: What to Expect Before,…
- How Much Does Medicare Pay For Outpatient Surgery:…
- How Much Does Aflac Pay for Outpatient Surgery: Find Out!
- What is Ambulatory Surgery? - Everything You Need to Know