As an Internal Medicine Physician, every day presents a unique tapestry of medical mysteries, ranging from the common cold to the intricate and unusual. One particular memory stands out — it was a sweltering summer afternoon when one of my patients shuffled in with severe abdominal pain. His face was etched with discomfort, and his case set me off on a journey to unravel the mystery of his pain and, in the process, discover the fascinating world of incarcerated hernias.
Hernias: A Simple Analogy

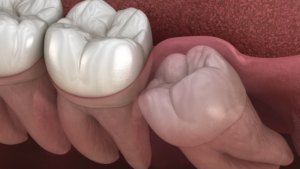
Imagine a busy highway with heavy traffic. Now picture a small section of the road, weakened by wear and tear, leading to a pothole. This is similar to what happens in our bodies. A hernia occurs when an organ pushes through an opening in the muscle or tissue that holds it in place. In my patient’s case, his intestine was the unruly traveler, and his abdominal wall was the compromised road.
Hernias are quite common, and they usually aren’t life-threatening. However, they do not go away on their own and may require surgical intervention to prevent complications.
Types
Hernias are classified into several types, depending on their location in the body:
- Inguinal: These occur in the inner groin.
- Femoral: These happen in the upper thigh/outer groin.
- Incisional: These occur through an incision or scar in the abdomen.
- Umbilical: These form at the belly button.
- Hiatal: These happen inside the abdomen, along the upper stomach/diaphragm.
Each type has its unique manifestation and requires different approaches for treatment.
Incarcerated Hernias: A Dangerous Turn
In most cases, hernias can be pushed back into their original place without much trouble, a term medically referred to as “reducible.” However, for my patient, this wasn’t the case. His hernia had become “incarcerated” — a condition where it can’t be pushed back into its original location. This occurs when a section of the intestine or fatty tissue gets trapped and is unable to slide back, leading to severe pain, discomfort, and potentially dangerous complications.
Incarcerated type represents a more serious progression of a typical hernia and, if left untreated, can lead to life-threatening situations.
Strangulated Hernias: The Critical Stage
One such perilous situation is when an incarcerated hernia evolves into a “strangulated hernia.” This is when the blood supply to the incarcerated organ or tissue is cut off. This can lead to the death of the affected tissue, causing severe pain and leading to serious complications, such as gangrene or peritonitis, which are potentially life-threatening if not treated immediately.
The urgency of the situation becomes evident here, as this type of condition requires immediate surgical intervention.
Diagnosing Process

Physical Examination
When my patient presented with severe abdominal pain, the first step was a physical examination. Often, an incarcerated hernia presents as a tender, hard lump in the abdomen or groin. The patient may also have symptoms like nausea, vomiting, fever, or sudden pain that worsens over time. However, diagnosing an incarcerated hernias can be challenging, as the symptoms can often mimic other abdominal conditions.
A careful physical examination can provide vital clues to the right diagnosis.
Imaging Studies
Imaging studies like X-rays, CT scans, or ultrasounds are often used to confirm the diagnosis of an incarcerated hernia. These images provide a detailed view of the internal structures, enabling doctors to identify the exact location and severity of the hernia. In my patient’s case, a CT scan was instrumental in confirming the presence of an incarcerated hernia.
These diagnostic tools help us not just in confirming the diagnosis but also in planning the appropriate treatment strategies.
Treatment
Non-Surgical Interventions
In some cases, non-surgical interventions like manual reduction, where a doctor tries to gently massage the hernia back into place, might be attempted. However, this is typically not the preferred approach for incarcerated hernias due to the risk of causing injury to the trapped tissue.
Remember, not all hernias are the same, and each case requires a personalized approach to treatment.
Surgery: The Gold Standard
Surgery is the primary treatment for incarcerated hernias. Depending on the patient’s overall health and the severity of the condition, this can be done as open surgery or laparoscopic surgery. In both types, the basic principle is to return the displaced organ to its original position and repair the defect in the muscle or tissue. In my patient’s case, an emergency laparoscopic surgery was performed, effectively treating his incarcerated hernia.
Prompt surgical intervention can prevent severe complications and offer the best chance for recovery.
Prevention and Long-Term Management

Lifestyle Changes
While hernias aren’t completely preventable, some lifestyle changes can reduce the risk:
- Maintain a healthy weight: Obesity increases abdominal pressure and the risk of hernias.
- Eat a high-fiber diet: This helps prevent constipation and straining during bowel movements.
- Avoid heavy lifting: If it’s unavoidable, use proper lifting techniques.
- Quit smoking: Smoking weakens the abdominal wall.
The importance of these small changes cannot be overstated in reducing the risk of hernias.
Follow-Up Care
Following successful treatment, patients need to be mindful of their recovery. Regular follow-ups with the healthcare provider are important to ensure the hernia has not recurred. Light exercises, as advised by the physician, can help strengthen the abdominal muscles.
Life After Surgery
Recovery and Rehabilitation
Post-surgery, patients like mine undergo a recovery phase. This can range from a few weeks to a couple of months, depending on the nature of the hernia and the individual’s general health. Pain management, wound care, and gradually resuming daily activities are critical components of this period.
During the recovery process, patients should adhere to the prescribed medication regimen, avoid lifting heavy objects, and report any unusual symptoms like fever, increased pain, or wound infection to their doctor promptly.
Importance of Physical Therapy
Physical therapy plays a vital role in recovery from hernia surgery. Specific exercises aimed at strengthening the abdominal wall and improving core stability are incorporated into the rehabilitation process. However, these should be done under professional supervision and only when the surgeon gives the go-ahead to avoid complications.
Physical therapy helps in a smoother transition back to daily activities and reduces the risk of hernia recurrence.
Psychological Impact

Mental Health Matters
It’s important to address that an incarcerated hernia can have significant psychological implications. Living with constant, intense pain can cause anxiety and depression, affecting a patient’s overall quality of life. In my patient’s case, the pain and subsequent surgery had a profound impact on his mental well-being.
Ensuring access to mental health resources and offering emotional support is an integral part of comprehensive care.
Role of Support Groups
Support groups can offer emotional support and practical advice to patients going through similar experiences. They provide a platform for individuals to share their journey and learn from others who have undergone similar experiences. Hearing about others’ experiences and tips for managing recovery can be comforting and reassuring during difficult times.
Remember, physical health and mental health are two sides of the same coin, both requiring equal attention and care.
Research and Future Directions in Treatment
Technological Advancements in Hernia Repair
Research and innovation are paving the way for advanced treatment options in hernia repair. Developments in surgical techniques, like robot-assisted surgery, provide more precision and less invasiveness. Furthermore, advances in materials used for hernia mesh are leading to better patient outcomes and lower recurrence rates.
These advancements hold great promise for even better patient outcomes in the future.
Toward Personalized Medicine
Just like every patient is unique, the approach to their hernia treatment should be as well. This is the concept of personalized medicine – tailoring the treatment plan to the individual patient’s characteristics. By considering factors such as the patient’s genetic makeup, lifestyle, and the specific characteristics of their hernia, we can potentially create treatment plans that are more effective and have fewer side effects.
Ultimately, the goal is to shift from a one-size-fits-all approach to a more personalized one that ensures the best outcomes for each patient.
Final Words

In the end, my patient’s story was a testament to the strength of the human spirit and the profound impact of prompt medical intervention. His journey through the maze of an incarcerated hernia serves as a potent reminder for us all to listen to our bodies and seek timely medical attention.
Incarcerated hernias, while serious, can be effectively treated with the right care. Knowledge, as they say, is power. Being aware of our bodies, understanding the symptoms, and seeking help when something feels off – that’s the key to conquering medical mysteries.